Abstract
Background: Frontline therapy of Hodgkin lymphoma (HL) is strictly stage-adapted. Staging systems used are based on historical variables which only indirectly reflects tumor load (Ann Arbor stage) or lymphoma cytokine activity (systemic symptoms, erytrocyte sedimentation rate). With new, abbreviated interim PET-tailored chemotherapy schemes (2+2) and reduced radiotherapy protocols, there is a clinical need for precise staging tools. Last years have brought new insight into the prognostic role of metabolic quantitative PET parameters and HL-associated biomarkers. Total metabolic tumor volume (TMTV) measured using fluoro-deoxyglucose PET (FDG-PET) was found to be a predictor of therapy failure after frontline treatment (Kanoun 2014). Interestingly, TMTV was found capable of identifying poor responders within one (intermediate) staging group (Akhtari, 2018; Cottereau 2018). Serum concentrations of thymus and activation-regulated chemokine (TARC) and other cytokines have been proved to have prognostic significance in the patients treated both in the frontline and relapse setting (Moskowitz, 2015; Guidetti 2017). A relationship between pretreatment TMTV, baseline cytokines levels, and current staging systems has not been analyzed yet.
Aim: To analyzed quantitative metabolic PET parameters and selected soluble biomarkers in the context of the staging systems used in the U.S. and Europe
Methods: We have analyzed a prospectively enrolled cohort of forty-eight patients with HL who were diagnosed in two large university medical centers from 5/2015 to 2/2018. All pts have undergone pretreatment FDG-PET/CT with quantitative analysis of TMTV, Total Lesion Glycolysis (TLG), Maximum Standardized Uptake Volume (SUVmax.) and the Largest Tumor Diameter (LD) and were sampled for cytokine analysis within 16 (median) days from the PET/CT. We have analyzed a set of four serum biomarkers: CD30 (sCD30), CD163 (sCD163), TARC, and interleukin 6 (sIL6), which were measured using ELISA assays.
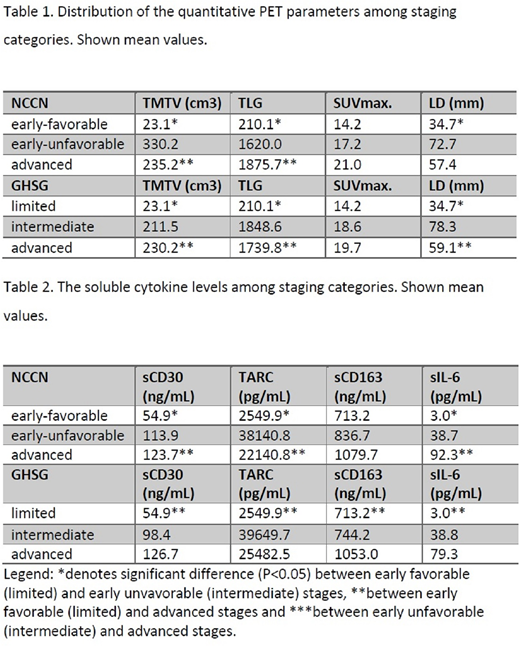
Results: A cohort consisted of 22 males and 26 females with median age of 42 years (range 21-75). Histology subtype was known in all but one case: nodular sclerosis in 23, mixed cellularity 15, lymphocyte-rich in 5 and nodular-lymphocyte predominant (NLPHL) in four. Ann Arbor stages were as follows: I in 5, II in 20, III in 13 and IV in 10 of the pts with systemic symptoms in 20 (42%) of them. All pts were classified according to the German Hodgkin Study Group (GHSG) and NCCN staging systems. GHSG stages - limited, intermediate and advanced were seen in 8 (17%), 10 (21%) and 30 (62%) pts, respectively. NCCN stages were distributed into early favorable in 8 (17%), early unfavorable in 17 (35%) and advanced in 23 (48%) of the pts. Chemotherapy was applied in all but four pts using: BEACOPPesc, combined BEACOPP+ABVD, ABVD and ABV/COPP protocols in 7, 15, 16 and six pts respectively. Of four pts without chemo one case was treated with local radiotherapy and three with WaW (all of them with NLPHL). Treatment response was known in 41 (85%) of the cases with CR, PR, and PD in 33 (80.5%), 6 (14.6%) and two (4.9%) pts, respectively. Relationships between disease stages and PET-parameters are summarized in Table 1. Briefly, metabolic tumor burden (TMTV, TLG) identified two markedly different groups: low and intermediate/high risk. Similarly, cytokines levels were significantly lower in low-risk patients compared to those with intermediate-high risk (Table 2). Treatment outcome did not correlate either with GHSG nor NCCN stage. We found correlation of sIL-6 (p=0.03) but not sCD30 (p=0.09), sCD163 (p=0.14) and TARC (p=0.57) with CR achievement. In terms of PET-parameters the high TMTV>104 cm3 (P=0.046) and TLG>798 (P=0.003) were associated with not achieving of CR with NPV, PPV and test accuracy of 94.4, 22.0, 58.5 for TMTV and 100%, 36,4%, 66% for TLG, respectively.
Conclusion: Adequate frontline treatment policy is vital for achieving an optimal balance between efficacy and toxicity. Current staging systems have a weak correlation with metabolic tumor burden: one-third of those recognized as advanced stage have the low burden, and vice versa about a half of intermediate-risk pts have high tumor burden. Combination of TMTV/TLG and cytokines can be currently used for decision making in borderline stage cases and probably could serve as a backbone for a new staging system in the future.
Acknowledgment: IGA_LF_2018_004, MH CZ-DRO (FNOL, 00098892)
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.